
Percuss across the abdomen as for flank dullness, with the point of transition from tympany to dullness noted.This maneuver is performed with the patient supine.Note: The tympany over the umbilicus occurs in ascites because bowel floats to the top of the abdominal fluid at the level of the fluid meniscus. Positive test: Percussion note is tympanitic over the umbilicus and dull over the lateral abdomen and flank areas.The location of the transition from tympany to dullness is noted.Direct percussion is done over the abdomen, from the umbilicus to the flanks.The patient is examined in the supine position.Note: A patient with an obese abdomen may also have flanks that bulge, although the fat of obesity extends further posterior than fluid in the peritoneum. Positive test: simply the presence of bulging flanks.With the patient supine, the examiner visually observes whether the flanks are pushed outward (presumably by large amounts of ascitic fluid).No single maneuver is both highly sensitive and specific therefore at least two maneuvers are necessary to increase the accuracy of physical exam for ascites. There are several physical examination maneuvers described for detection of ascites described below that are at least moderately sensitive and specific. Other techniques involve different patterns of the scratching, for example as in spokes of a wheel and other places for placing the stethoscope such as over the abdomen. One is to place the diaphragm over the area of the liver and then scratch parallel to the costal margin until the sound intensity drops off marking the edge of the liver. Several different techniques have been described for this exam. Palpate the bottom margin of the liver for the texture of the liver, i.e. Feel for the liver to hit the caudal aspect of your palpating hand. The liver will move downward due to the downward movement of the diaphragm. Palpate for the liver with one or two hands palm down moving upward 2-3 cm at a time towards the lower costal margin. Palpationīegin palpation over the right lower quadrant, near the anterior iliac spine. You can also use palpation to determine the lower border. Measure the vertical distance from the top to the bottom. Start in the lower right quadrant so as to not miss a greatly enlarged liver. Repeat the same process from below, moving again from resonance over the bowel to dullness and again mark the area of change. Percuss with the middle finger of your dominant hand on the middle finger of your non-dominant one.īegin percussion over the lungs and move from the area of resonant lung sounds to the areas of dullness. Place your non-dominant hand palm down flat on the abdomen with the fingers parallel to the lower costal margin pointed toward the midline. Percuss for the upper and lower margins of the liver. Listen over the area of the liver for bruits or venous hums. Auscultationįollow the inspection of the liver, as with the rest of the abdominal exam, with auscultation.
EXCESS ABDOMINAL FLUID SKIN
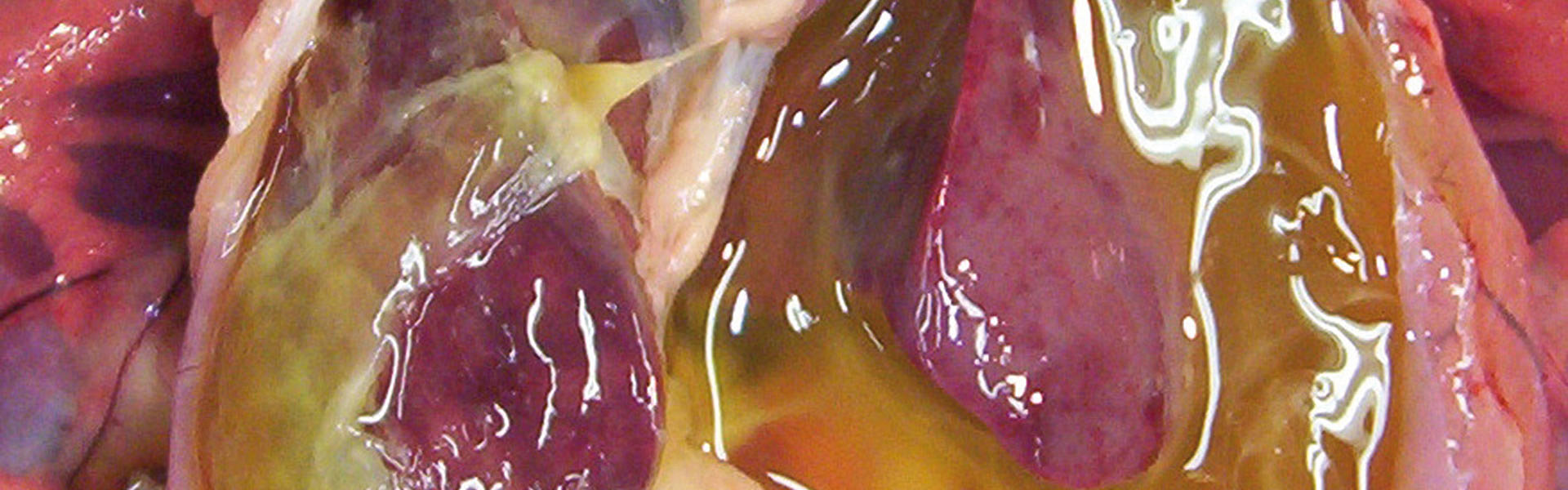
Look at the skin for signs of liver disease, such as caput medusa, or spider angiomata. Look for gross asymmetries across the abdomen. Additionally make sure your hands are warm so as to not startle the patient. For the best exam, make sure the patient is warm and comfortable. Preserve the patient’s privacy by draping the top of their body with the gown and below the waist with a sheet. All rights reserved.] Techniques: Liver & Ascites Technique: LiverĪpproach the examination of the liver from the right side of the patient. Nurse clinicians are capable of reducing mortality in intra-abdominal hypertension and abdominal compartment syndrome patients by incorporating the latest evidence in fluid resuscitation techniques.Ībdominal compartment syndrome Capillary leak Colloid Crystalloid Damage control resuscitation Fluid resuscitation Intra-abdominal hypertension Third spacing.Ĭopyright © 2017 Elsevier Inc. Careful consideration is necessary when achieving fluid balance in acutely ill patients, including reducing the use of crystalloids, implementing damage control resuscitation, and establishing measurable resuscitation endpoints. Intra-abdominal hypertension and abdominal compartment syndrome are deadly complications of third spacing and capillary leak that occur secondary to excessive fluid resuscitation. Excessive resuscitation with crystalloids places patients at particular risk for many subsequent complications that carry associated increases in mortality and morbidity. Fluid resuscitation is a primary concern of nurse clinicians.


 0 kommentar(er)
0 kommentar(er)
